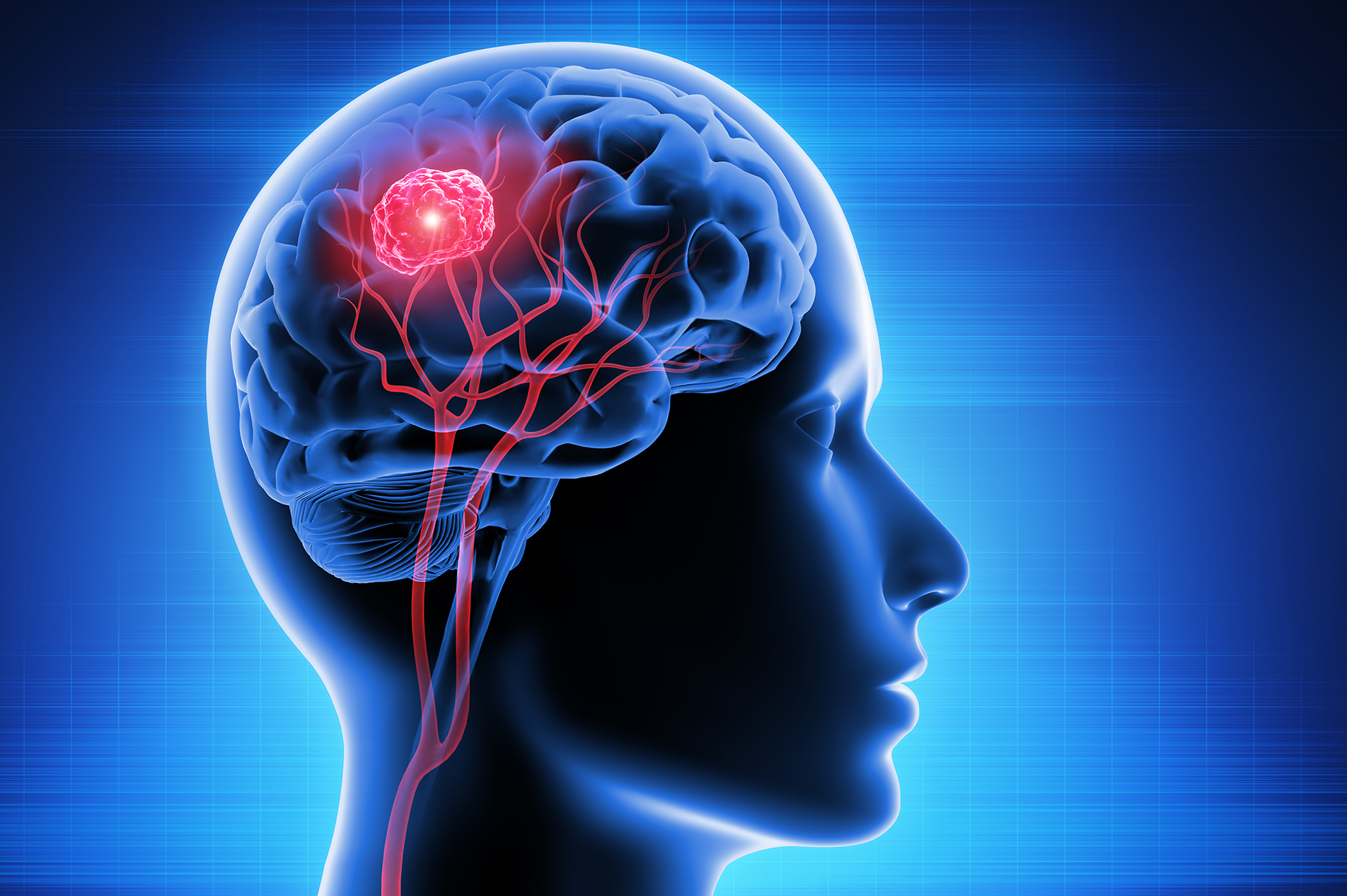
Stereotactic radiosurgery can eradicate brain tumors without a single incision. Johnathan A. Engh, MD, neurosurgeon with Lexington Brain and Spine Institute and Joshua D. Lawson, MD, with Lexington Radiation Oncology explain how the treatment works and the benefits it provides patients.
What is stereotactic radiosurgery?
Stereotactic radiosurgery is a non-invasive method of radiation administration that uses imaging to precisely deliver x-rays to either eliminate or stop the growth of various tumors. The technique is best known for treating conditions of the brain, but various forms of stereotaxy are also used for precise radiation treatment elsewhere in the body.
What types of brain tumors can be treated using this technology?
The most common tumors treated with radiosurgery are metastases. These are cancerous tumors that develop elsewhere in the body and move through the bloodstream to the brain.
Other tumors commonly treated with radiosurgery include meningiomas, vestibular schwannomas (also known as acoustic neuromas) and some gliomas, to name a few.
What are the advantages of radiosurgery vs. craniotomy?
Unlike a craniotomy, in which the skull is opened to surgically remove a tumor, radiosurgery requires no surgical scar so there is no risk of wound infection or bleeding. Radiosurgery does not require anesthesia and can be performed as an outpatient. In addition, radiosurgery can treat multiple tumors in one setting, which is generally not feasible via craniotomy.
Patients who have a craniotomy frequently need a break from their chemotherapy treatments to heal from surgery. Stereotactic radiosurgery patients almost never need a break from chemotherapy treatments.
Compared to whole brain irradiation, radiosurgery has a very benign side effect profile. In fact, a large proportion of patients have no side effects at all. And radiosurgery has been shown to have better cognitive outcomes than whole-brain irradiation in both the short term and the long term.
What else do you want readers to know about stereotactic radiosurgery?
Radiosurgery, when properly applied, is both very safe and highly effective. However, no one treatment is always right. The best way to determine the optimal course of treatment for each patient is through a multidisciplinary care team.
At Lexington Medical Center Brain Tumor Program, we see patients together in our multidisciplinary clinic and assess each individual patient for potential treatment options of stereotactic radiosurgery, standard radiation therapy, medical treatment, open surgery, or no treatment at all. We also have a close working relationship with our medical oncologists, to make sure that our treatments are coordinated in an ideal fashion. Our team has physicians have each performed hundreds, if not thousands, of stereotactic radiosurgery treatments and is committed to the highest clinical standards.

Johnathan A. Engh, MD, FAANS, Lexington Medical Center Brain and Spine Institute,
Lexington Medical Center Brain Tumor Program

Joshua D. Lawson, MD, Lexington Radiation Oncology,
Lexington Medical Center Brain Tumor Program






Leave a comment