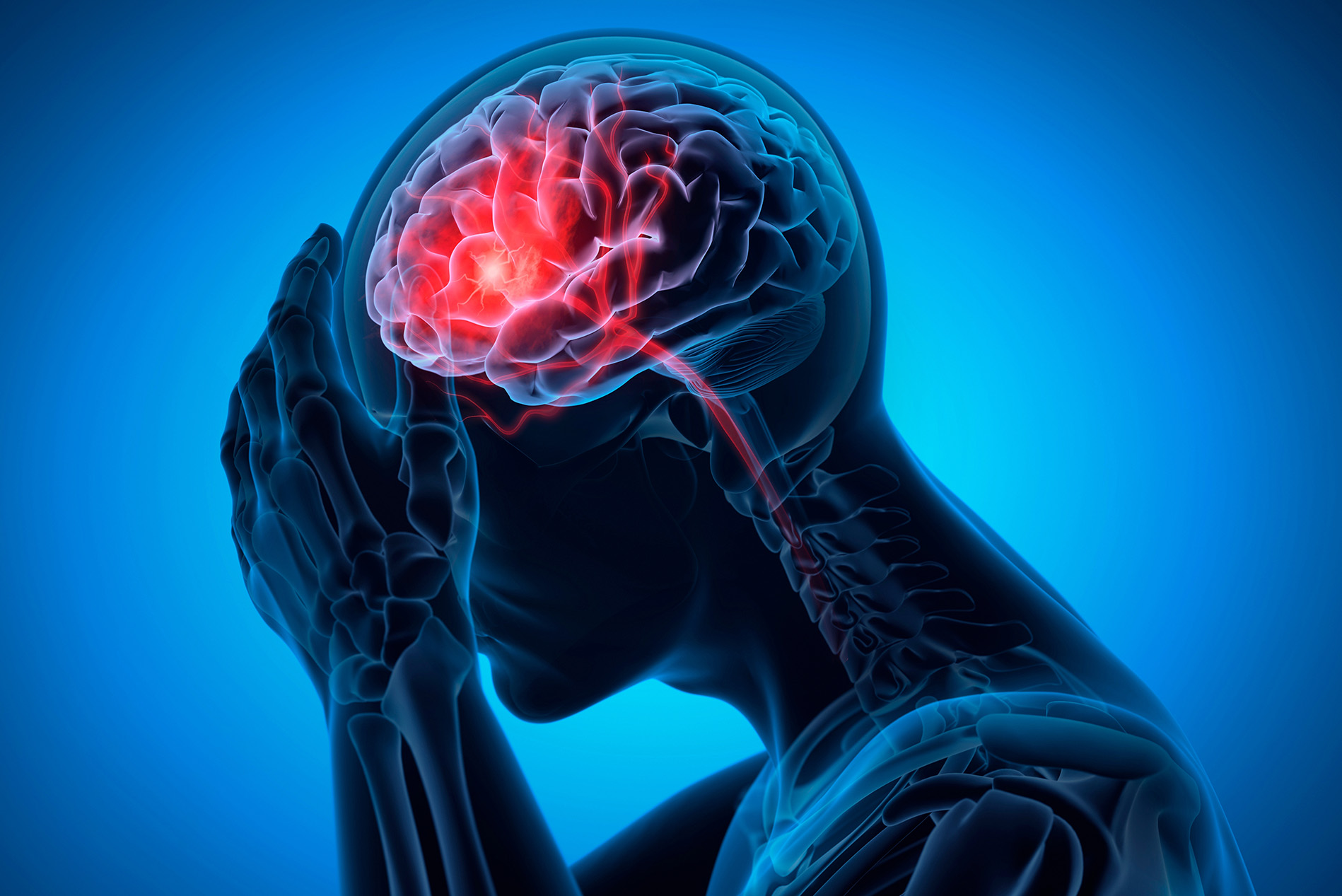
A stroke is a serious and significant medical emergency. Unfortunately, it's an all-too-common one as well. According to the South Carolina Department of Public Health (SCDPH), strokes were responsible for 20,879 trips to the ER in 2022 (the most recent year for which data is available). As our population ages, the problem only gets bigger.
So, what exactly is a stroke?
"Stroke occurs when a part of the brain is starved of oxygen and blood and undergoes dysfunction," said Frank Pusey Jr., MD, neurologist and medical director of the Stroke Program at Lexington Medical Center. "That can happen because a blood vessel either gets clogged up or ruptures."
"We see at least two or three stroke alerts per day in our hospital. It's very common, particularly in the Southeast, and this state," says Dr. Pusey. "There are several reasons for that, including genetics. There's a high number of patients with high blood pressure and diabetes. We are a heavy-smoking population, and so there are some lifestyle issues we deal with as well."
Age also comes into play.
"The older we get, the higher our risk for stroke," Pusey explained. "And the longer you have high blood pressure, your risk of stroke increases over time. The biggest thing to worry about is the damage that particularly high blood pressure can cause to the blood vessels themselves, and diabetes, of course. And then over time, that gets worse, increasing the risk for stroke."
Since stroke is so prevalent and its consequences so severe, it's important to be on the lookout for its warning signs. That's where a handy acronym, 'BE FAST' comes into play.
'BE FAST' stands for...
Balance: Is the person suddenly having trouble with balance or coordination?
Eyes: Is the person experiencing sudden blurred or double vision - or a sudden loss of vision in one or both eyes without pain?
Face Drooping: Does one side of the face droop, or is it numb? Ask the person to smile to check.
Arm Weakness: Is one arm weak or numb? Ask the person to raise both arms. Does one arm drift downward?
Speech Difficulty: Is speech slurred, or is the person unable to speak or difficult to understand? Ask the person to repeat a simple sentence like, "The sky is blue." Is the sentence repeated correctly?
Time to call 911: If the person shows any of these symptoms (even if the symptoms go away), call 911 and get them to the hospital immediately.
That last point is especially significant, Dr. Pusey noted. Since stroke is the fifth-leading cause of death in the United States, responding immediately once warning signs appear is critical. Rapid response to stroke can mean the difference between life and death.
"Time is very critical," Dr. Pusey noted. "We say 'time is brain.' The longer the stroke goes on, the more damage it can do. Also, we have treatments and acute interventions that we can do, but they're very time-constrained. We have to get a patient into the hospital very quickly to use these clot-dissolving drugs. They're most effective within the first four and a half hours after a stroke begins. The quicker we get it into the patient's system, the more effective it is in limiting the damage in the long run."
"The other option that we have beyond that window is if we see a clot in the blood vessel in the brain, we can occasionally take a catheter, slide it where that clot is, and remove it," Dr. Pusey continued. "We can do that for up to 23 hours. But again, the sooner we do all this and we open that blood vessel, the better opportunity we have for improvement in the long run."
Afterward, therapy can help patients who have suffered certain types of stroke in their recovery.
"Rehab is very essential, Dr. Pusey said. "With us, it starts on day one. Rehab outside of the hospital situation depends on how severe the stroke is. Some patients can do it at home, while others need to go to rehab. I believe the more intensive the rehab, the better. And that sometimes requires a patient to go to an inpatient rehab facility."
Depending on the situation, rehab can include physical, occupational, and speech therapy.
On the front end, there are several steps you can take to help lower your risk of stroke.
"If you have a history of high blood pressure, diabetes, and cholesterol, then as tightly as you control those particular diseases, the better off you are going to be," Dr. Pusey advised. "Certain lifestyle changes - like good, healthy eating, good oral hygiene and good sleep habits - can also lower the risk factors for stroke. Being treated for sleep apnea is also helpful. And certainly, we don't want patients smoking cigarettes or drinking to excess."
But should a stroke happen, Dr. Pusey has one critical message for all of us to remember.
"The main thing we want people to remember is if they have a stroke, recognize the symptoms, and then BE FAST," Dr. Pusey concluded. "Don't go to urgent care. Don't try to drive. Call 911 and get yourself here. Don't try to wait for it to go away or see what happens."

Frank O. Pusey, Jr., MD, Lexington Hospitalists






Leave a comment