by Brett B. Fowler, MD, Lexington Medical Heart & Vascular Center
Deep vein thrombosis (DVT) is a serious medical condition affecting hundreds of thousands of Americans annually. Blood clots that travel through the venous system, known as venous thromboembolism, is the third leading cause of cardiovascular death, behind heart attack and stroke. DVT is the most common cause of preventable death in the U.S.
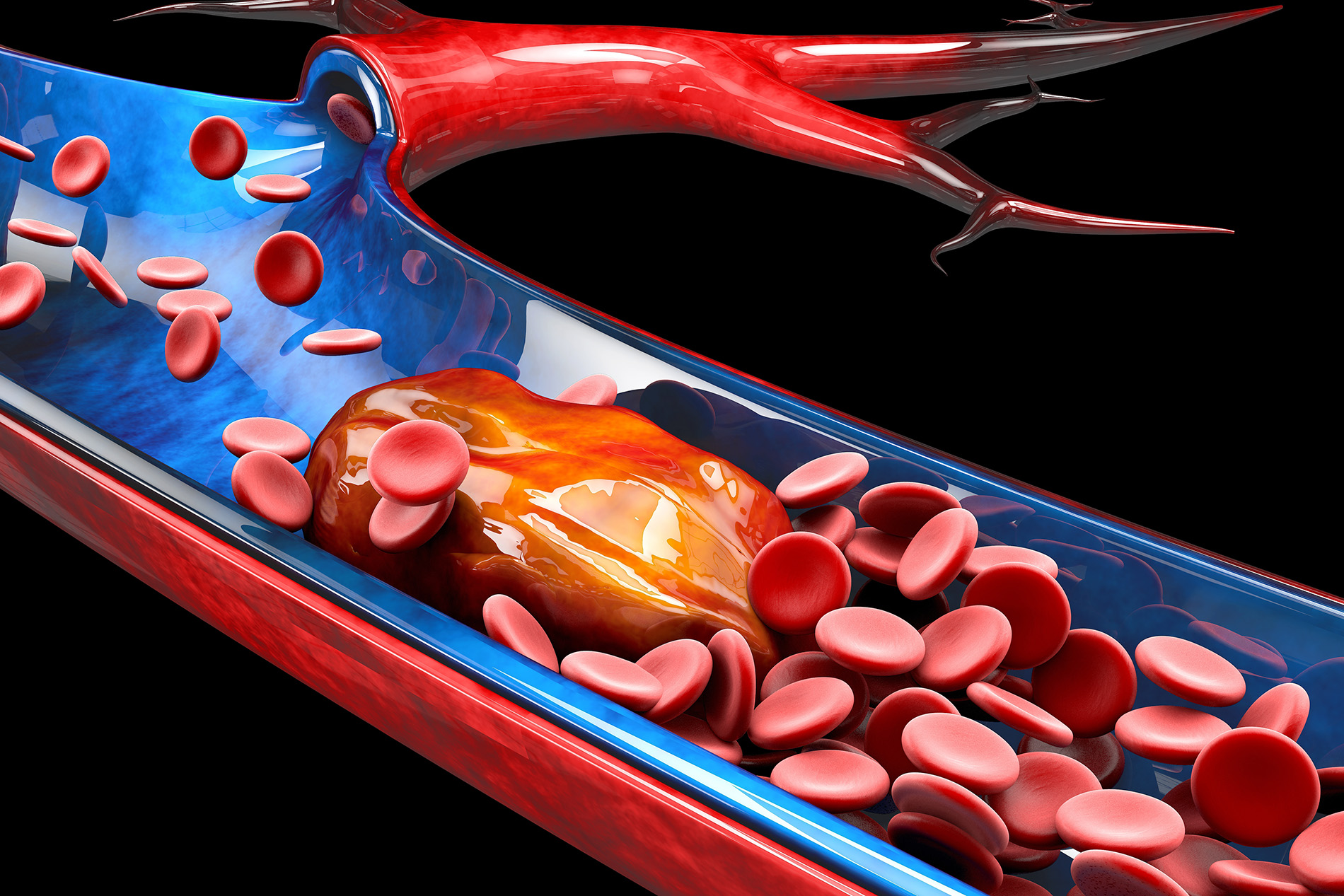
What is a DVT?
A DVT is a blood clot that forms in the body's veins. Veins are responsible for the drainage and return of blood back to the heart. DVTs most commonly form in the veins of the legs but can also involve the arms and the deeper veins of the chest and abdomen. DVTs can range from small clots in a single vein or involve an extensive network of veins. Some clots can break loose and travel to the lungs, called a pulmonary embolus (PE), a medical emergency.
What are the risk factors of DVT?
There are many risk factors in the development of DVTs, including:
- Smoking
- Obesity
- Age >60
- Immobilization
- Cancer
- Recent surgery or trauma
- Family history of blood clots
- Hormone therapy
- Pregnancy
- History of prior DVT
What are the symptoms of a DVT?
Patients often complain of pain, swelling and discoloration of the affected extremity. More worrisome signs include numbness of the skin, muscle weakness or development of wounds.
DVTs are first suspected on physical exam, and the diagnosis is confirmed with duplex ultrasound studies that visualize clots in the veins. Additional laboratory studies and imaging may be required, such as a CT scan or MRI.
What can I do to prevent a DVT?
Staying active is essential. The veins of the legs require muscle movement to assist the blood return to the heart. Avoid smoking, as tobacco use can increase your risk of clotting. Talk to your doctor about any family history of blood clots or use of hormone therapies, including birth control, to discuss your risks of developing blood clots. On long flights or road trips, stay hydrated, take frequent breaks to walk around, and consider using compression socks or stockings. If you are hospitalized, on bedrest or undergoing surgery, your doctor may prescribe blood thinners to reduce your risk of DVT.
What is the treatment for a DVT?
The vast majority of DVTs are treated with anticoagulation, which is also known as blood thinners. Compression therapy with stockings or wraps and elevation of the affected extremity can reduce and improve your symptoms. In rarer cases of extensive or obstructing DVT, your doctor may need to perform a procedure to remove the clot called a thrombectomy or inject medication into the clot to dissolve it called thrombolysis.

Brett B. Fowler, MD, vascular surgeon at Lexington Medical Heart & Vascular Center








Leave a comment