Mar 1, 2024, 8:58 AM
by
Allison Sanford
Spinach is not only as a staple in various cuisines, but it also is a symbol of strength and health. Packed with nutrients, it stands out as a must-have superfood for any health-conscious person.
Feb 28, 2024, 4:44 PM
by
Allison Sanford
With urgent care clinics and telemedicine options readily available, younger generations may not see the need for a primary care physician. But there are better ways to care for your health than relying on urgent care.
Feb 28, 2024, 4:42 PM
by
Allison Sanford
Watch the first episode of HealthCast, our new video series. This episode features the innovative technology Lexington Medical Center offers to treat blood clots that has better outcomes and a faster recovery time than blood thinners.
Feb 27, 2024, 1:59 PM
by
Allison Sanford
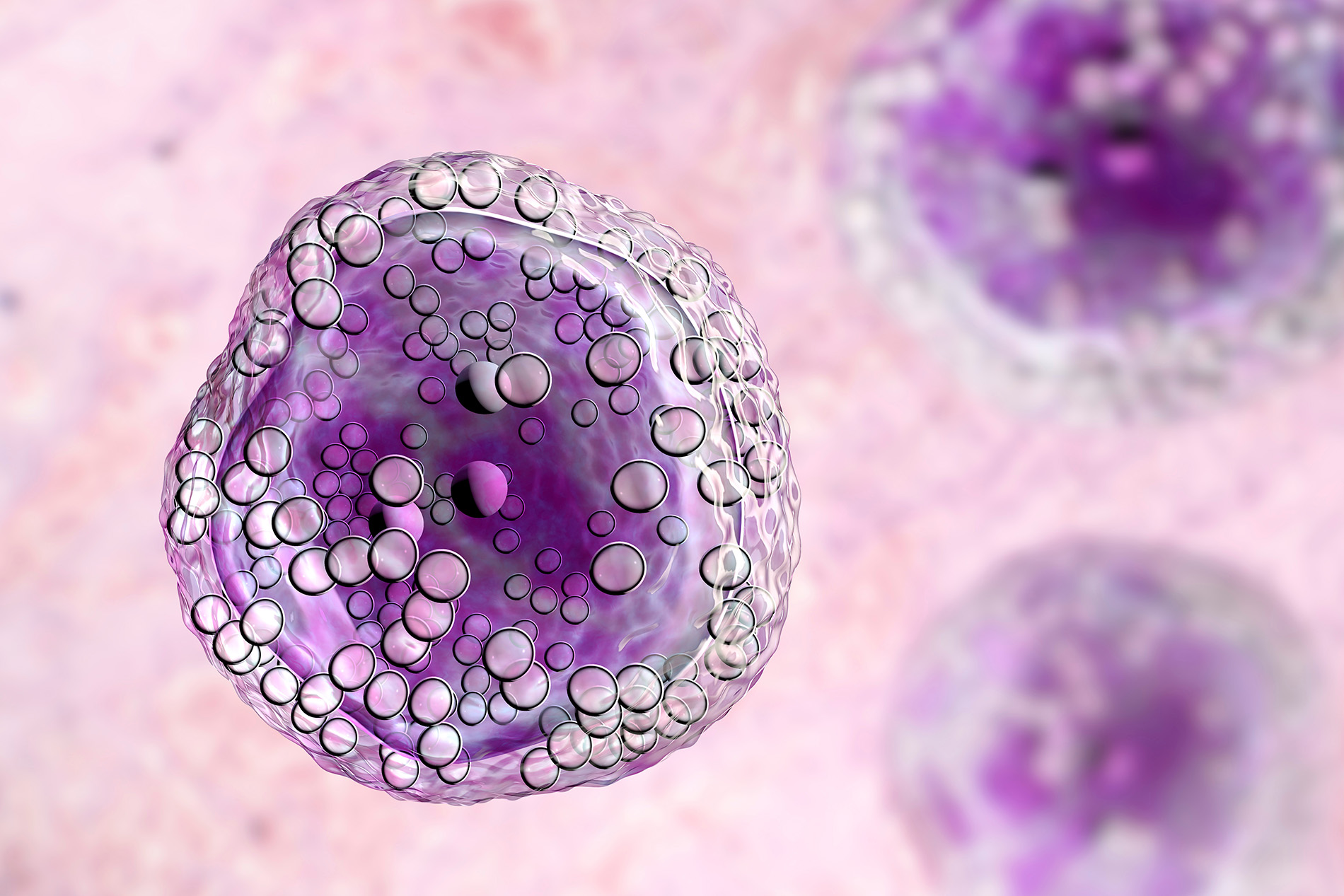
Lymphoma is a broad term for cancer that begins in cells of the lymphatic system, which is part of the body's germ-fighting network.
Feb 19, 2024, 9:59 AM
by
Allison Sanford
Abnormal uterine bleeding as any unexpected or irregular bleeding from the uterus that deviates from your normal menstrual cycle pattern. It includes bleeding that is heavier in volume, lasts longer, or occurs outside the usual menstrual cycle.
Feb 6, 2024, 10:01 AM
by
Allison Sanford
Adopting a heart-healthy lifestyle can overcome genetic predispositions and pave the way for a longer, healthier life.
Feb 5, 2024, 1:43 PM
by
Allison Sanford
While many of us may associate heart care with older age, the truth is that it's never too early to start prioritizing cardiovascular health.
Feb 1, 2024, 3:42 PM
by
Allison Sanford
Despite its tiny size, quinoa is mighty in nutrition and versatility. It’s a wholesome choice to boost your diet with a nutritious, plant-based protein.
Jan 29, 2024, 9:51 AM
by
Allison Sanford
Infertility is a challenge no couple wants to face, but one in six couples has trouble conceiving.
Jan 26, 2024, 2:00 PM
by
Allison Sanford
Lots of things change with age, including your eyesight. If you're starting to notice blurry vision, it could be the start of macular degeneration.



![ScreenShot for Blog[62] Steve and Mamie Turner on the beach with their dog](https://blog.lexmed.com/images/librariesprovider80/blog-post-featured-images/screenshot-for-blog-62.jpg?sfvrsn=36ab6f0a_0)
![shutterstock_1674223735[41] Smiling middle aged woman riding a bicycle](https://blog.lexmed.com/images/librariesprovider80/blog-post-featured-images/shutterstock_1674223735-41.jpg?sfvrsn=9f546f0a_0)





.jpg?sfvrsn=dd1f6f0a_0)
.jpg?sfvrsn=b91c6f0a_0)




